The Dictionary of Sydney was archived in 2021.
Hospitals
Citation
Persistent URL for this entry
To cite this entry in text
To cite this entry in a Wikipedia footnote citation
To cite this entry as a Wikipedia External link
Hospitals
[media]Hospitals in Sydney are represented by their buildings, often large imposing structures suggesting solid permanence. Historically, it is a misleading impression, as hospitals have been among the most changeable European institutions transplanted to Australia. In Sydney the first hospital was basically for the military and prisoners; hospitals later became charitable institutions for the sick poor, and finally medical institutions. [1]
The first hospitals
In 1788, the First Fleet not only brought imperial notions of conquest, but naval surgeon John White as head of the new medical service. The assumption was that, as a penal colony, the state would provide rudimentary healthcare for its sailors, soldiers and prisoners. White and four medical assistants almost immediately set up tents at the newly (re)named Dawes Point at The Rocks. The tents, Australia's first hospital, were replaced some months later by the first hospital building, designed for up to 80 patients. In 1790 this building was itself replaced with a prefabricated wood and copper hospital structure, brought to the colony by the Second Fleet. From the time of the Second Fleet, hospitals also provided care for increasing numbers of free settlers. [media]As European occupation extended, public hospitals were built west of the original settlement of Sydney: at Parramatta, Windsor and Liverpool. Initially, hospital care was also extended to some Aboriginal people, though it did little to help the Cadigal people cope with the smallpox epidemic of 1789, nor to alleviate the subsequent devastation of Aboriginal life. [2]
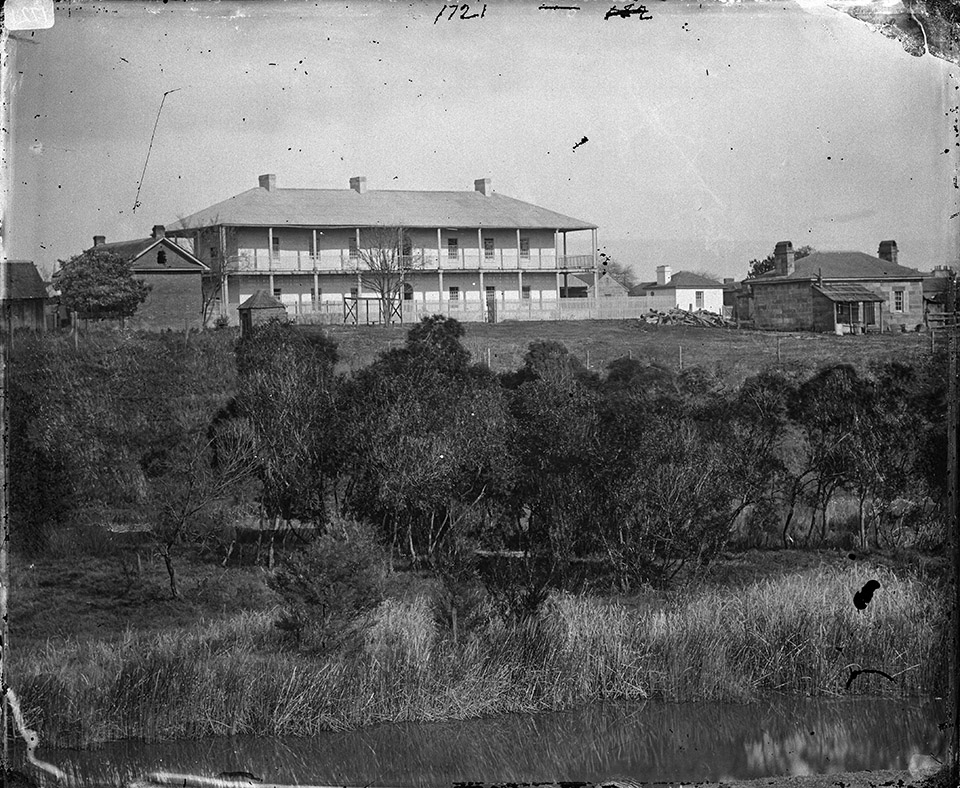
It did not take long for persistent problems to emerge. One of the first was a lack of equipment and beds, particularly in times of crisis or epidemics. The first major medical crisis affecting the white population came with the arrival of the Second Fleet. It disembarked so many sick convicts that the hospital was crammed to capacity and still some 100 tents were needed for all the patients. By 1810, when Governor Lachlan Macquarie arrived in the colony, the need for new military and general hospitals was urgent. [media]By 1815 Macquarie had a new military hospital built on Observatory Hill. It lasted until 1850 when the military was transferred to Victoria Barracks at Paddington.
The 'Rum Hospital'
Macquarie also found an ingenious solution to fund the building of a new general hospital. He granted to three colonists a short-term but lucrative monopoly on importing spirits in exchange for them building the new hospital in Macquarie Street. [media]Consequently, the Sydney Infirmary and Dispensary (from 1881, Sydney Hospital) was nicknamed the 'Rum Hospital'. It opened in 1816 with one large central and two smaller wings. Today the northern wing houses the New South Wales state parliament and the southern wing is The Mint building. The large central segment caused intractable problems until its demolition in 1876. Its foundations were inadequate, causing problems with damp and subsidence, and its walls were built from rubble that provided an ideal home for rats, bedbugs and other vermin. [3]
From its beginning, Sydney Hospital demonstrated how dependent hospitals are on the quality of their staff and the powers allotted to their managers. [media]The first surgeon in charge of the new Macquarie Street hospital was the ex-mutineer William Redfern. Although he was known as a skilled surgeon, the hospital was notoriously chaotic. In contrast, his successor, the naval surgeon James Bowman, 'performed miracles' by enforcing order and attempting to provide systematic care. Bowman's successors, including James Mitchell, generally did their best with limited resources. Despite this varied history, popular accounts of Sydney Hospital still assume that its care was always callous and chaotic until the introduction of trained nurses, under Lucy Osburn, in 1868. [4]
Improving hospital care
Another common misconception is that the poor quality of early hospital care was always viewed as a problem. What is forgotten about the key public hospitals in Sydney that admitted civilians is that until the 1840s they mainly catered for convicts and ex-convicts, with nursing care provided by other convicts and convalescent patients. Expectations of adequate care only marginally increased after transportation ceased and, from 1848, the general hospitals focused on patients who were 'paupers' (dependent on charity or government welfare) or impoverished. The overwhelming majority of the population paid to receive medical, surgical and nursing care at home. A dominant fear in the Australian colonies, as in Britain, was of 'pauperism': that providing too high a level of service to those claiming government or private charity would lead to permanent dependency. The response was to try to provide humane care but not at a level which made the services attractive. As a result, Sydney hospitals, like their British counterparts, tended to be feared as places of pain where patients faced lonely deaths away from family and friends. [5]
[media]Two factors, apart from humanitarianism, helped to improve the basic standard of care provided. One was the system of financing public hospitals. The colonists believed charitable works, including public hospitals, should be privately financed. They had an intense fear of replicating anything approaching the English Poor Law with its dreaded workhouses and associated infirmaries. In practice, hospitals were expensive to run and only a small proportion of their cost was met by private donations. To stimulate charitable giving, private subscribers to the hospital funds were allowed to recommend the admission of a certain number of patients per year. Many employers subscribed in order to provide cheap healthcare for their servants and other employees, but demanded at least an adequate level of care. [6]
The second practical factor in ensuring a minimal level of humanity in hospitals was the need to provide care for accident victims, many of them injured in industrial accidents. If possible, accident patients were taken to their own homes but many were admitted to accident wards. The first casualty (emergency) department was established at Sydney Hospital around 1870. Demand for hospital casualty services increased from 1895, with the introduction of an ambulance service in Sydney. From the 1920s Sydney hospitals experienced a surge in demand from the middle class as well as their traditional poorer patients. This demand came from victims of accidents involving the increasing numbers of cars (initially poorly designed for safety), trams and motorbikes. [7]
Religious hospitals
Hospitals were also established to demonstrate religious philanthropy. During the twentieth century these religious hospitals became major providers of hospital care in Sydney, open to patients of any, or no, religion. There were two practical motives for this openness: to attract general community support and to qualify for government subsidies which were not granted to 'sectarian' charities.
[media]The first of the denominational hospitals was St Vincent's Hospital, founded by the Sisters of Charity in 1857 at Potts Point (it moved to its present site at Darlinghurst in 1870). The sisters' motives were humanitarian but also aimed to ensure that dying Catholic patients could do so safely within their church's rituals. Later, other Catholic nursing orders established hospitals, most notably the Sisters of Mercy's Mater Misericordiae at North Sydney, founded in 1906.
Protestant denominations generally did not feel the need to found their own hospitals, but one enduring exception is the Lottie Stewart Hospital at Dundas, founded by the Wesley Mission of the Methodist Church in 1948. The Seventh Day Adventist Church, despite its minority status, founded the highly successful Sydney Sanitarium Hospital which opened in Wahroonga in 1903 with 70 beds. Now the Sydney Adventist Hospital, it cares for around 40,000 inpatients and 150,000 outpatients annually. Sydney's first Jewish hospital, the Wolpers Hospital, was established in 1948 and still operates in Woollahra. [8]
Avoiding 'hospitalism'
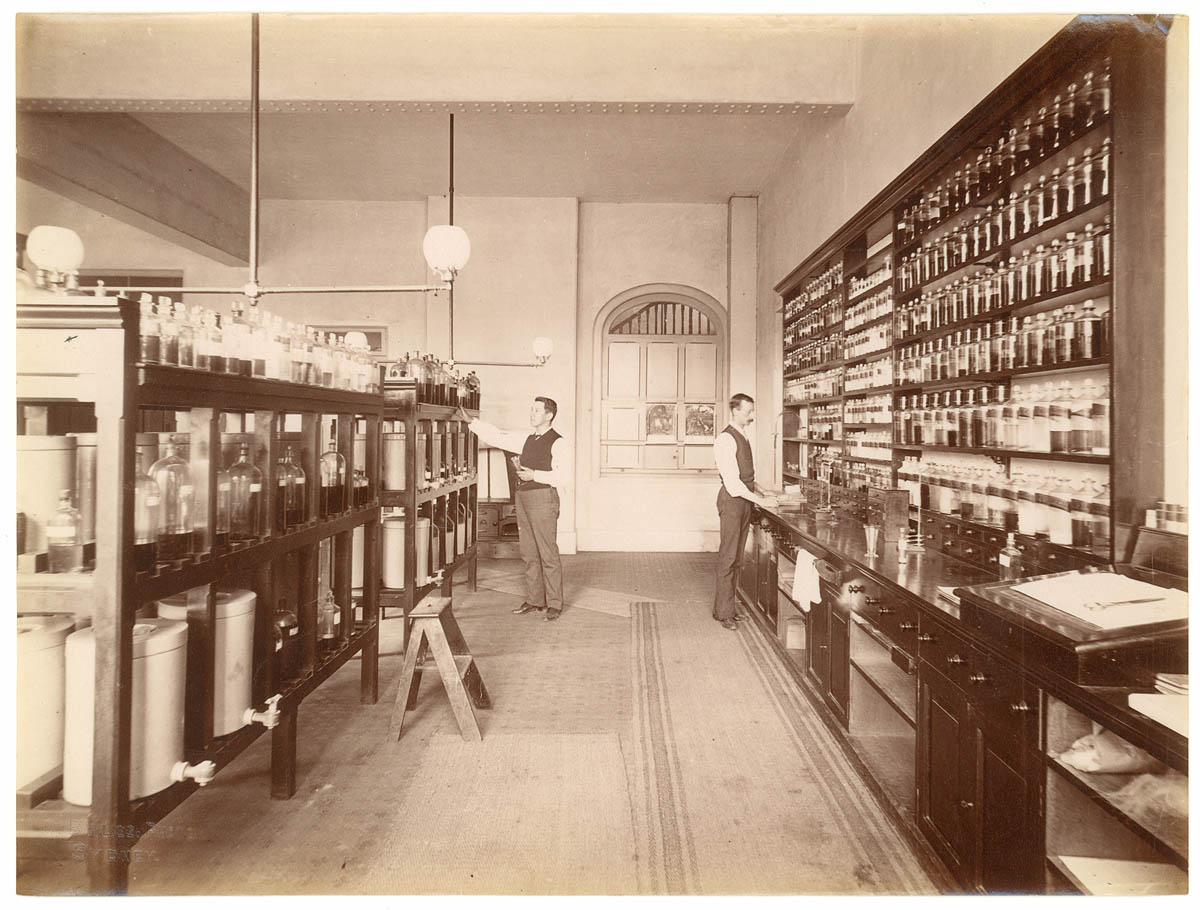
Before the 1860s, there was little incentive for even the sickest, poorest patient to be admitted to a hospital. For most of the nineteenth century, one of the strongest deterrents was the fear of 'hospitalism'. Hospitalism was the explanation for rampant infections within hospitals and was understood as toxic 'miasmas', vapours which seeped into the walls of hospitals and let off fumes which caused disease. Despite their fear and low expectations for care, many patients had no choice but to enter a hospital when sick. Sydney Hospital remained by far the largest public hospital, its patient numbers swollen by patients admitted from country areas. During 1871, in a colony of some 500,000 Europeans, Sydney Hospital had 1,840 patient admissions. In comparison, Parramatta and Windsor hospitals had 76 and 52 admissions respectively and St Vincent's had 289. The importance of Sydney Hospital is even greater when outpatients are considered. [media]The Dispensary at Sydney Hospital was founded in 1826 and in 1871 it serviced 5,972 'paupers'. St Vincent's cared for 500 paupers and Windsor hospital only 33. No outpatient service was provided at Parramatta. [9]
Effective medicine arrives
Sydney hospitals, like hospitals in other British settlements, began to change fundamentally from the mid-nineteenth century. Gradually and unevenly they ceased to be healthcare charities and became medical institutions catering for all sections of the population. One historian, David Wootton, concluded that if medicine is the ability to cure disease, then 'there was very little medicine before 1865'. It is a dramatic way of emphasising how western medicine and western hospitals were transformed around this time.
From the 1840s onwards, more effective patient therapies were introduced, with an emphasis on improved nutrition and replacing vital fluids, rather than the traditional reduced diets, enemas and blood-letting through leeches. A flurry of innovations and inventions followed, including the use of anaesthetics in surgery, hypodermic syringes, improved clinical thermometers and stethoscopes. Capping it all from the 1860s was the gradual and uneven acceptance of the existence of germs and of Joseph Lister's antiseptic techniques to destroy germs in surgical incisions and other wounds. By the 1890s aseptic technique was common, attempting to prevent germs from entering the body in the first place. [10]
Specialising hospital care
[media]From the late nineteenth century, Sydney hospitals routinely employed trained nurses and increasingly offered effective cure and care. Medical and nursing training schools and specialities developed in response to advances in medical science. The middle class quickly realised the new benefits of hospitals. They paid to enter the increasing number of private and intermediate wards in public hospitals and also provided a steady clientele for the numerous private hospitals scattered around Sydney. [11] Mirroring this change of function, Sydney's public hospitals were controlled, not by philanthropic businessmen as before, but by boards strongly influenced by senior doctors. Medical superintendents began to be routinely appointed, and doctors who devoted part of their practice to hospital patients on an honorary basis wielded considerable power.
From the 1880s, specialised and suburban public hospitals were founded to meet the increasing demand for hospital care and the increasing specialisation of medicine. In that decade alone, the following hospitals were opened: Sydney Eye Hospital (Moorcliff) at Millers Point; Sydney Hospital for Sick Children in Glebe (later the Royal Alexandra Hospital for Sick Children at Camperdown, and now the Children's Hospital at Westmead); (later Royal) Prince Alfred Hospital at Camperdown; The Coast (later Prince Henry) Hospital; and the North Shore Cottage (later the Royal North Shore) Hospital.
The Coast Hospital was a rare example of the colonial government intervening directly to meet a particular healthcare need. It began, like Sydney Hospital, as a series of tents. [media]The tents housed victims of the 1881 smallpox epidemic and were located in then-remote Little Bay in southeastern Sydney. It soon became a permanent facility for patients with infectious diseases. The North Shore Cottage Hospital illustrates the trend for small suburban hospitals to expand in size and complexity during the twentieth century. Two other examples of this transition from a small hospital housed in a 'cottage' to a large complex are Kogarah's St George Hospital, founded in 1894, and Manly Hospital, founded in 1896. [12]
Improvements in hospital-based obstetrics and gynaecology were slower to be implemented. [13] [media]One women's hospital, the Rachel Forster Hospital, deserves mention because of its unique genesis for Sydney and its demonstration of the essential role that public hospitals still play in medical training. It was founded in 1922 in Redfern by six female doctors as a response to the difficulty they had in gaining hospital experience. Specialist women's hospitals like the Rachel Forster were generally closed or amalgamated as a result of the trend to larger hospitals during the late twentieth century. The largest, Crown Street Women's Hospital, closed in 1983 and the Rachel Forster Hospital closed in 1996. [14]
[media]Another hospital which deserves special mention is the Sydney Homoeopathic Hospital, founded in 1902 at Redfern, and moved to Glebe in 1915. It was distinctive because it rejected conventional medicine and was one of a string of homeopathic hospitals founded throughout Australia at the turn of the century. The hospital mirrored the quick decline in popularity of homeopathy and effectively ceased such treatment in 1945, though the hospital itself did not close until 1989. Commitment to the homeopathic approach to medicine did not entirely die, and the year after the hospital closed, a homeopathic outpatient clinic was opened at Balmain Hospital that still operated part-time in 2008. [15]
From charity to citizen's right
Fred Flowers, the Labor minister for health in New South Wales, announced in 1911 that public hospital care was no longer a charity but a citizen's right. As this view was slowly accepted, governments demanded, and eventually won, a greater say in hospital management. In 1929 Sydney's public hospitals came under the control of the Hospitals Commission of New South Wales while private hospitals were regulated by the Board of Health. Building on highly controversial efforts by the Chifley government, the Commonwealth government also increased its control, in exchange for providing hospital subsidies, with the National Health Act (1953).
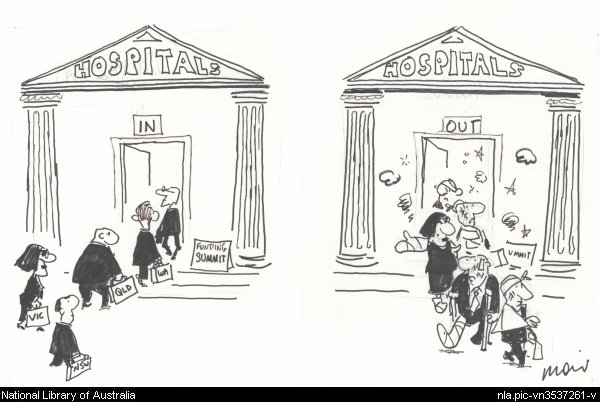
[media]After the election of the Whitlam Labor federal government in 1972, hospital funding became a festering political dispute. Different versions of national health insurance schemes came and went as governments changed. Government encouragement of private health insurance helped to encourage the formation of private hospitals, many of them operating in conjunction with public hospitals. Federal and state governments continue to argue over funding. In 2007–08, news stories about substandard conditions in Sydney's public hospitals indicate that funding levels and divided responsibility remain major problems. [16]
The mid-twentieth century was the golden age of medical dominance of hospitals. Senior doctors assumed god-like status within 'their' hospitals. Nurses were expected to display primary loyalty to the hospital that trained them and to defer to the idiosyncrasies of each doctor and ward sister. Patients rarely questioned or complained. Medical advances continued to make hospitals more effective, particularly the discovery of sulpha drugs in 1935 and the manufacture of penicillin in Australia from 1944. Though neither proved to be the elusive 'magic bullet' to cure all infections, these and other antibiotics helped to transform Sydney hospitals and save countless lives. Vaccination programs, improved public health and better nutrition all boosted general health and reduced or eliminated the need for hospitals to cater for regular epidemics, particularly of childhood infections. [17]
The golden age was never quite as golden as many believed. The twin functions of public hospitals as providers of patient care and sites for medical and nursing education could result in conflicting priorities. Despite heroic efforts by some individuals and organisations, some patients were always neglected, most notably Indigenous Australians. The new drug therapies and specialised medicine became increasingly expensive, placing immense strain on hospital budgets. From the late twentieth century, hospitals also struggled to deal with diseases associated with affluence, sedentary lifestyles and increased longevity. As Sydney's population spread, hospitals were no longer in the best locations for patients. New hospitals only partially met the needs of the new centres of population. These new hospitals in western Sydney included Nepean (1956 at Kingswood), Blacktown (1965), Westmead (1978), and Mt Druitt (1982).
Staffing troubles
From the mid-twentieth century, hospital staffing became increasingly difficult, gradually affecting even the most prestigious Sydney hospitals. The early discharge of patients meant that only the sickest stayed in hospital, which, along with the emergence of antibiotic-resistant strains of bacteria, made care by students increasingly dangerous. From the 1940s a chronic shortage of nurses jeopardised the ability of hospitals to function and resulted in periodic ward closures. In 2008, a projected shortage of medical staff also has serious implications for future hospital staffing. [18]
A further complication is that as hospital care became more complex and specialised, it increasingly involved coordinating not just the medical, nursing and domestic staff but up to 17 other healthcare occupations, including medical imaging professionals, physiotherapists, occupational therapists, social workers and hospital pharmacists. Hospitals became too large and complex to continue with a simple model of medical dominance. The importance and power of honorary doctors declined, and from the 1940s professional managers were increasingly appointed. With these changes have come attempts to change hospital culture. One aspect which remains a serious concern is the conviction that working while dangerously sleep-deprived is a necessary 'rite of passage' for junior hospital doctors. Another concern is the length of time before the occasional 'rogue' doctor is prevented from continuing an unsafe practice. [19]
Amalgamations
By 1985 problems largely related to cost meant that the smaller Sydney public hospitals were 'in fear of their lives'. Sydney Hospital was one hospital which mounted a long series of diverse and passionate campaigns in order to survive, albeit as a small facility amalgamated with the Sydney Eye Hospital. Many hospitals were less successful and closed or merged with other hospitals. [media]The result is huge complexes such as the one around the Prince of Wales Hospital at Randwick, which absorbed the Prince Henry, Royal South Sydney and Eastern Suburbs Hospitals and includes the Royal Hospital for Women (previously at Paddington) and the Sydney Children's Hospital (previously the Prince of Wales Children's Hospital).
Religious hospitals were not immune from the trend, with, for example, the Sisters of Mercy's Mater Misericordiae Hospital merging in 2001 with the Sisters of Charity's St Vincent's Private and Public Hospitals, Darlinghurst.[media] Other hospitals, such as the Concord Repatriation Hospital, founded in 1941 to care for military veterans, broadened their scope to include general admissions. The administration of Sydney hospitals followed a similar pattern, with hospital boards being replaced by area health services. In 2008 Sydney public hospitals are managed through four large area health services, each of which also covers regions beyond greater Sydney. [20]
Sydney hospitals in 2008 had little in common with the first hospital tents erected in 1788. Yet, despite all the problems and changes, their outstanding characteristics have been the loyalty they engender in staff and the generally high regard of the public. The crucial test, which hospitals have passed for most of the last century, is that most people in Sydney, when sufficiently ill, see hospital care as their best option.
Notes
[1] State Records New South Wales, Archives in Brief 57 – Hospital buildings
[2] John White, Journal of a Voyage to New South Wales, http://gutenberg.net.au/ebooks03/0301531.txt (accessed March 2008); Brian Dickey, 'Health and State in Australia, 1788–1977', Journal of Australian Studies, 2, November 1977, pp 50–63; Sydney, circa 1803, from the western side of the cove, painting attributed to GW Evans; Inga Clendinnen, Dancing with Strangers, Text Publishing, Melbourne, 2003, pp 216, 275
[3] HYPERLINK "http://www.seahs.nsw.gov.au/publichealth/introduction/history.asp" http://www.seahs.nsw.gov.au/publichealth/introduction/history.asp citing letter by John White, 4 July 1788 (accessed November 2007); JHL Cumpston, Health and disease in Australia: a history, Milton Lewis (ed), Australian Government Publishing Service, Canberra, 1989, pp 38–41; Noel McLachlan, 'Macquarie, Lachlan (1762–1824)', Australian Dictionary of Biography, vol 2, Melbourne University Press, Melbourne, 1967, pp 187–195; Judith Godden, Lucy Osburn, a Lady Displaced. Florence Nightingale's Envoy to Australia, Sydney University Press, Sydney, 2006, especially chapter 4; http://www.teachingheritage.nsw.edu.au/3readings/site_ob1.html (accessed March 2008)
[4] Edward Ford, 'Redfern, William (1774–1833)', Australian Dictionary of Biography, vol 2, Melbourne University Press, Melbourne, 1967, pp 368–371; Nancy Gray, 'Bowman, James (1784–1846)', Australian Dictionary of Biography, vol 1, Melbourne University Press, Melbourne, 1966, pp 137–138; Elizabeth Guilford, 'Mitchell, James (1792–1869)', Australian Dictionary of Biography, vol 2, Melbourne University Press, Melbourne, 1967, pp 235–238. Susanne de Vries, The Complete Book of Great Australian Women, Harper Collins, Sydney, 2003, pp 346–55
[5] Valerie Griffiths, From Tents to Stone, the author, Coffs Harbour, New South Wales, 2005; Brian Dickey, No Charity There. A Short History of Social Welfare in Australia, Thomas Nelson, Melbourne, 1980; Anne O'Brien, Poverty's Prison: The Poor in New South Wales 1880–1918, Melbourne University Press, Melbourne, 1988
[6] Judith Godden, Lucy Osburn, a Lady Displaced. Florence Nightingale's Envoy to Australia, Sydney University Press, Sydney, 2006, pp 42–45; JHL Cumpston, Health and Disease in Australia: a History, Milton Lewis (ed), Australian Government Publishing Service, Canberra, 1989, pp 116,132,176–78
[7] Elizabeth Harford, 'Blood, Antiseptics and Stale Beer. The History of the Development of Casualty Nursing in Sydney, 1870–1939', PhD thesis, University of Sydney, 2003, pp 10, 218, 370–77
[8] Michael Horsburgh, 'Government Subsidy of Voluntary Social Welfare Organisations: A Case Study NSW 1858–1910', Master of Social Work thesis, University of New South Wales, 1975; Hilary Carey, In the best of hands: a history of the Mater Misericordiae Public Hospital & the Mater Misericordiae Private Hospital, North Sydney, 1906–91, Hale and Iremonger, Sydney, 1991 and L Heath, L and P Curthoys, Lottie Stewart Hospital 1948–1998, Lottie Stewart Hospital, Sydney, c 1997; Sydney Adventist Hospital, http://www.sah.org.au/events.press.details.asp?sku=955792884; Wolpers Hospital, http://www.join.org.au/media/wolper.htm (both accessed March 2008)
[9] Brian Dickey, 'Health and State in Australia, 1788–1977', Journal of Australian Studies, 2, November 1977, pp 50–63; Inga Clendinnen, Dancing with Strangers, Text Publishing, Melbourne, 2003, pp 216, 275; Ann Mitchell, Pictorial Guide to the History of Sydney Hospital, Sydney Hospital, Sydney, 1978, p 1 (unpaginated); NSW Statistical Register, 1871, p 8.
[10] David Wootton, Bad Medicine: Doctors Doing Harm Since Hippocrates, Oxford University Press, Oxford, 2006, p 281; Carol Helmstadter, 'Early Nursing Reform: A Doctor-Driven Phenomenon', Medical History, 46, 2002, pp 325–50; Mary Poovey, Uneven Developments: The Ideological Work of Gender in Mid-Victorian England, University of Chicago Press, Chicago, 1988; Michael Worboys, Spreading Disease: Disease Theories, and Medical Practice in Britain, 1865–1900, Cambridge University Press, New York, 2000; Susan Hardy, 'Surgical Spirit. Listerism and the Medical Profession in NSW, 1867–1889', PhD thesis, University of New South Wales, 1990
[11] Hazel Woolston, 'The Growth of Private Hospital System in Metropolitan Sydney from 1884 to 1932', Master of Arts thesis, University of Sydney, 1986
[12] Don Hamilton, Hand in Hand: the Story of the Royal Alexandra Hospital for Children, Sydney, John Ferguson, Sydney, 1979; Bruce Storey et al, Royal Prince Alfred Hospital, 125 Years, Royal Prince Alfred Hospital, Sydney, 2007; Geoffrey Sherington with Roger Vanderfield, The Royal North Shore Hospital, 1888–1988: a Century of Caring, Horwitz Grahame, Sydney, 1988; Sue Rosen, 'Conservation Plan for The Prince Henry Hospital, Little Bay', Sue Rosen and Associates, Sydney, 1990; Maylean Cordia, Nurses at Little Bay, Prince Henry Hospital Trained Nurses' Association, Sydney, 1990; http://www.sesiahs.health.nsw.gov.au/sgh/about_sgh/history.asp (accessed March 2008); Pauline Curby, Visitor's Sixpence: Manly Hospital The First 100 Years, Manly Hospital and Community Health Services, Sydney, 1996; Northern Beaches Health Service, http://www.nscchealth.nsw.gov.au/services/003700641.shtml
[13] Lisa Featherstone, 'Birth in Sydney', Sydney Journal, vol 1, no 1, March 2008, pp 20–26
[14] Royal Hospital for Women, From Charity to Choice. The History of the Royal Hospital for Women, (video) South East Sydney Area Health Service, c 1997; Ian Cope and William Garrett, The Royal. A History of the Royal Hospital for Women, 1820–1997, Royal Hospital for Women, Sydney, 1997; State Records New South Wales, 'Archives in Brief 88 – Crown Street Women's Hospital'; Louella McCarthy, 'All this fuss about a trivial incident? women, hospitals and medical work in New South Wales, 1900–1920', Women's History Review, vol 14 no 2, 2005, pp 267–85; Louella McCarthy, 'Women Doctors and a Sense of Place', Public History Review, 9, 2001, pp 45–60; and Louella McCarthy, 'Idealists or Pragmatists? Progressives and Separatists among Australian Medical Women, 1900–1940', Social History of Medicine, vol 16, no 2, 2003, pp 263–282
[15] http://www.homeopathyoz.org/downloads/Hist-NSWHomHosp-Sydney.pdf (accessed 2008); Philippa Martyr, Paradise of Quacks. An Alternative History of Medicine in Australia, Macleay Press, Sydney, 2002, pp 143, 241
[16] Sydney Morning Herald, 11 March 1911, cited in Brian Dickey, 'Health and State in Australia, 1788–1977', Journal of Australian Studies, 2, November 1977, pp 50–63; State Records New South Wales, Concise Guide to the State Archives (H–K): Hospitals Commission; Sidney Sax, A Strife of Interests, Politics and policies in Australian health services, George Allen and Unwin, Sydney, 1984; http://www.abc.net.au/news/stories/2007/11/19/2094289.htm (accessed December 2007); http://www.pm.gov.au/media/interview/2008/interview_0092.cfm (accessed March 2008)
[17] Robert Evans, 'The Transformation of Australian Hospitals between the 1940s and the 1970s', http://www.historycooperative.org/journals/hah/7.2/evans.html (accessed November 2007); Evan Willis, Medical Dominance: the Division of Labour in Australian Health Care, revised edition, Allen and Unwin, Sydney, 1989; Kathryn Hillier, 'Babies and bacteria: Phage typing, bacteriologists and the birth of infection control', Bulletin of the History of Medicine, vol 80 no 4, Winter 2006, pp 733–61
[18] Peter Brooks et al, 'Medical Workplace Issues in Australia: "tomorrow's doctors – too few, too far"', Medical Journal of Australia, 179, 2003, pp 206–08
[19] Mary Harris, Paul Gavel and Warwick Conn, 'Planning Australia's hospital workforce', Australian Health Review, vol 25 no 5, 2002, pp 61–77; Antony Nocera and Diana Khursandi, 'Doctors' working hours: can the medical profession afford to let the courts decide what is reasonable?', Medical Journal of Australia, 168, 1998, pp 616–18
[20] 'Rachel Forster, Profile of a Community Service', The Lamp, August 1985, p 6; Northern Sydney Central Coast Area Health Service, www.nscchealth.nsw.gov.au; South Eastern Sydney and Illawarra Area Health Service, www.sesiahs.health.nsw.gov.au; Sydney South West Area Health Service, www.sswahs.nsw.gov.au; Sydney West Area Health Service, www.wsahs.nsw.gov.au (all accessed March 2008)
.